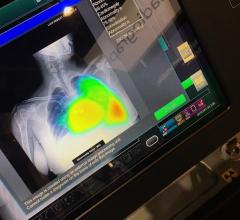
November 29, 2022 — Researchers have developed a deep learning model that uses a single chest X-ray to predict the 10-year risk of death from a heart attack or stroke, stemming from atherosclerotic cardiovascular disease. Results of the study were presented today at the annual meeting of the Radiological Society of North America (RSNA).
Deep learning is an advanced type of artificial intelligence (AI) that can be trained to search X-ray images to find patterns associated with disease.
"Our deep learning model offers a potential solution for population-based opportunistic screening of cardiovascular disease risk using existing chest X-ray images," said the study's lead author, Jakob Weiss, M.D., a radiologist affiliated with the Cardiovascular Imaging Research Center at Massachusetts General Hospital and the AI in Medicine program at the Brigham and Women's Hospital in Boston. "This type of screening could be used to identify individuals who would benefit from statin medication but are currently untreated."
Current guidelines recommend estimating 10-year risk of major adverse cardiovascular disease events to establish who should get a statin for primary prevention.
This risk is calculated using the atherosclerotic cardiovascular disease (ASCVD) risk score, a statistical model that considers a host of variables, including age, sex, race, systolic blood pressure, hypertension treatment, smoking, Type 2 diabetes and blood tests. Statin medication is recommended for patients with a 10-year risk of 7.5% or higher.
"The variables necessary to calculate ASCVD risk are often not available, which makes approaches for population-based screening desirable," Dr. Weiss said. "As chest X-rays are commonly available, our approach may help identify individuals at high risk."
Dr. Weiss and a team of researchers trained a deep learning model using a single chest X-ray (CXR) input. They developed the model, known as CXR-CVD risk, to predict the risk of death from cardiovascular disease using 147,497 chest X-rays from 40,643 participants in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial, a multi-center, randomized controlled trial designed and sponsored by the National Cancer Institute.
"We've long recognized that X-rays capture information beyond traditional diagnostic findings, but we haven't used this data because we haven't had robust, reliable methods," Dr. Weiss said. "Advances in AI are making it possible now."
The researchers tested the model using a second independent cohort of 11,430 outpatients (mean age 60.1 years; 42.9% male) who had a routine outpatient chest X-ray at Mass General Brigham and were potentially eligible for statin therapy.
Of 11,430 patients, 1,096, or 9.6%, suffered a major adverse cardiac event over the median follow-up of 10.3 years. There was a significant association between the risk predicted by the CXR-CVD risk deep learning model and observed major cardiac events.
The researchers also compared the prognostic value of the model to the established clinical standard for deciding statin eligibility. This could be calculated in only 2,401 patients (21%) due to missing data (e.g., blood pressure, cholesterol) in the electronic record. For this subset of patients, the CXR-CVD risk model performed similarly to the established clinical standard and even provided incremental value.
"The beauty of this approach is you only need an X-ray, which is acquired millions of times a day across the world," Dr. Weiss said. "Based on a single existing chest X-ray image, our deep learning model predicts future major adverse cardiovascular events with similar performance and incremental value to the established clinical standard."
Dr. Weiss said additional research, including a controlled, randomized trial, is necessary to validate the deep learning model, which could ultimately serve as a decision-support tool for treating physicians.
"What we've shown is a chest X-ray is more than a chest X-ray," Dr. Weiss said. "With an approach like this, we get a quantitative measure, which allows us to provide both diagnostic and prognostic information that helps the clinician and the patient."
Co-authors are Vineet Raghu, Ph.D., Kaavya Paruchuri, M.D., Pradeep Natarajan, M.D., M.M.S.C., Hugo Aerts, Ph.D., and Michael T. Lu, M.D., M.P.H. Investigators were supported in part by funding from the National Academy of Medicine and the American Heart Association.
For more information: www.rsna.org


 October 08, 2025
October 08, 2025