
Nov. 11, 2014 — Shockwave Medical announced positive clinical results from Disrupt PAD trial, a single-arm multicenter study evaluating the safety and utility of Lithoplasty balloon catheters for the treatment of peripheral artery disease, at the Vascular Interventional Advances (VIVA) Annual Conference in Las Vegas, Nev.
In advanced vascular disease, atherosclerosis becomes calcified deep inside the vessel walls, limiting blood flow. These deposits are difficult to treat because they limit the effectiveness of current balloon angioplasty, making today’s interventions challenging and prone to both procedural and long-term failure. Lithoplasty is a novel balloon-based technology that utilizes integrated lithotripsy, a pulsatile mechanical energy commonly used to break up kidney stones, to disrupt both superficial and deep calcium and normalize vessel wall compliance prior to low-pressure balloon dilatation. Lithoplasty is designed to be naturally gentle to non-diseased portions of the vessel while remaining hard on calcium, the tissue that limits vessel expansion and the effectiveness of current technologies.
Early clinical evaluation from 35 patients with calcified vascular stenosis of the superficial femoral artery (SFA) and popliteal artery demonstrated safe and effective dilatation of calcified stenosis with no acute failures, favorable residual stenosis, and no re-intervention out to 30 days, with no major adverse events. Primary efficacy results demonstrated 100% success, defined as ability to achieve less than 50% residual stenosis using Lithoplasty with or without adjunctive angioplasty. Device success was 87%, defined as ability to achieve less than 50% residual stenosis using Lithoplasty alone. Importantly, an average residual stenosis of 23% (initial 76%), with no difference in the ability to dilate lesions between moderate (36%) and severely (64%) calcified lesions, was noted. Thirty-day patency assessed by duplex ultrasound was 100%.
First-In-Man Results Presented at TCT 2014
Results from the first-in-man study of five patients with moderate to severe coronary calcification presented in September at the annual TCT conference in Washington, D.C. demonstrated safety, tolerability, deliverability, and effectiveness for Lithoplasty as a pre-treatment of calcified coronary lesions prior to stenting.
“Disruption of calcium within the vessel wall with Lithoplasty enables the use of low balloon pressures to dilate lesions and improve blood flow. This has the potential to minimize barotrauma and soft tissue vascular injury common to traditional balloons and existing endovascular technologies — an exciting breakthrough for patients with difficult-to-treat coronary calcifications, which continues to be a major problem in cardiology today,” said Todd Brinton, M.D., co-founder of Shockwave Medical and clinical associate professor of interventional cardiology, Stanford University.
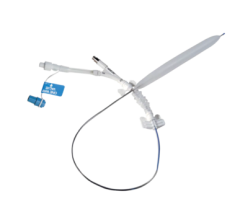
About Shockwave’s Lithoplasty System
Unlike current devices that treat only superficial calcium (angioplasty and athetectomy), Shockwave’s Lithoplasty system is designed to be effective on all types of calcium, including deep, which is the type known to limit vessel expansion. Delivered on a standard balloon catheter platform, Lithoplasty combines the calcium disrupting power of lithotripsy with the familiarity and simplicity of a balloon in a single enabling device. Lithoplasty applies a brief series of powerful mechanical pulses designed to safely travel through soft tissue, disrupt and pre-treat calcium. The integrated balloon is then dilated at low pressures to expand the lesion evenly, potentially minimizing acute soft tissue injury that could lead to the need for additional interventional treatments, or long-term restenosis. Early clinical results demonstrate safety, tolerability, deliverability and effectiveness for Lithoplasty as a treatment for patients with peripheral artery disease and as a pre-treatment of calcified coronary lesions prior to stenting. Shockwave has completed patient enrollment for a CE study of the technology in the peripheral vasculature. Clinical work has also been conducted in coronary vessels, and will begin in aortic valves next year.
For more information: www.shockwavemedical.com

 June 13, 2024
June 13, 2024 









