Many formerly invasive diagnostic and interventional cardiology procedures have migrated to less invasive or percutaneous options. The subsequent rise in cath lab procedures has increased the need for alternatives to manual compression that promote hemostasis at the access site, allowing for quicker patient ambulation and throughput. Noninvasive methods, most commonly used with diagnostic procedures, provide topical hemostasis at the puncture site, whereas invasive devices penetrate the skin to close the wound — often with a plug or suture — within or on top of the tissue tract.
Despite the variety of devices available, the goal is universal: to promote rapid hemostasis and reduce access site complications.
With manual compression only, depending on the size of the sheath, pressure had to be applied for 10-20 minutes and patients would have to remain sedentary for approximately three to six hours, explains Michael C. Kim, M.D., director of the coronary care unit and director of medical education in the cardiac catheterization laboratory at Mount Sinai Heart, New York, NY.
“With closure devices, complete hemostasis is achieved before the patient even leaves the cath lab, and when properly performed, there is no need for manual compression or intense monitoring of the groin site,” noted Dr. Kim.
Compared to first-generation devices, today’s closure devices are much simpler to deploy, which has contributed largely to their overall acceptance and use. For example, closure devices, such as the Angio-Seal (St. Jude Medical) and PerClose (Abbott Vascular), are used in more than 90 percent of the cases in Mount Sinai’s cath lab.
The Angio-Seal is an intravascular device that sandwiches the arteriotomy between a bio-absorbable anchor and collagen sponge, which dissolve within 60 to 90 days. Because a mechanical seal is created, hemostasis does not depend on clot formation. The device’s VIP (V-Twist Integrated Platform) technology reportedly provides a larger collagen footprint for better arteriotomy coverage and is designed for enhanced conformability around the artery for a more uniform and secure seal.
“The Angio-Seal boasts a very difficult to beat combination of safety, efficacy and ease of use in both diagnostic and angioplasty procedures,” said Dr. Kim. “It is the first device that gave a great majority of operators the confidence to use a closure device and feel comfortable with the results.”
However, for patients who are likely to return within three months for repeat procedures, Dr. Kim opts for the suture-based PerClose, explaining that it is easier to navigate a needle through a suture than around a collagen plug.
Wired for Success
Arizona Heart Institute (AHI), a center purely dedicated to cardiovascular surgery and endovascular procedures, performs approximately 3,000 vascular and endovascular procedures per year. All endovascular procedures, including diagnostic, are performed surgically in one of the four dedicated endovascular suites within the OR.
As closure device technology evolved and the devices became easier to use, AHI gradually migrated away from exclusive use of manual compression. Initially, the facility used suture-based devices but found these devices could cause extensive scarring, which hindered reopening of the groin for repeat angiograms or endoluminal grafts. In addition, leaving a foreign substance behind in the body — a hook, plug, staple or suture — raises the the risk of infection, according to Venkatesh Ramaiah, M.D., director of peripheral vascular surgery and endovascular research at AHI.
In Dr. Ramaiah’s opinion, the purpose of closure devices is three-fold: (1) they should safe and effective, (2) they should be usable in any kind of vessel structure and (3) they should not be prone to causing infection or causing an occlusion of the artery.
Today, physicians at AHI rely on the Boomerang system from Cardiva for 70 to 80 percent of their cases in the OR. They were drawn to the device’s principle advantage: No foreign material is left behind in either the vessel or subcutaneous tissue. It is also quick and easy to deploy and can be used in small vessels, even ones that are calcified, according to Dr. Ramaiah. But the biggest benefit, he says, is the Boomerang allows blood flow to be maintained while the closure device is still in place.
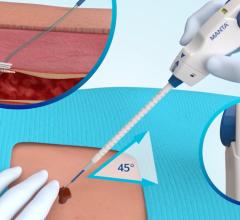
The system is comprised of the Boomerang wire that is inserted into the femoral artery through the existing introducer sheath; a flat, low-profile disc that contours to seal the arteriotomy; and a clip placed on the skin to create site-specific compression of the arteriotomy and tract, establishing hemostasis. Once the fascial tract recoils back to its predilated state and the blood coagulates, the disc is collapsed, the wire is removed and finger pressure is applied.
Dr. Ramaiah finds the Boomerang suitable for almost all procedures, including in brachial arteries, for antegrade and retrograde punctures and in grafts. But because the system is a two-step procedure, with the second step — removing the device and applying manual compression for five minutes — being performed by recovery room nurses, there was initially some resistance to the device. ”Why not use manual compression only?” they questioned.
“With the Boomerang, the amount and time of manual pressure is markedly decreased — by about 80 percent — versus manual compression alone,” explained Dr. Ramaiah, which could be reason enough to convince some doubters. But more importantly, he says, AHI’s studies report a zero infection rate associated with the Boomerang.
Fast ACTing Hemostasis
The University of Rochester Medical Center’s (Rochester, NY) full-service cath lab is staffed with six full-time faculty interventional cardiologists and performs more than 5,000 diagnostic and interventional procedures per year. Currently, the center is conducting a clinical trial involving the SafeSeal Hemostasis Patch from Possis Medical.
The noninvasive SafeSeal’s design is built on MPH (Microporous Polysaccharide Hemospheres) technology that reportedly facilitates dehydration of the blood cells, which concentrates and compresses cells, platelets and fibrin at the vessel access site.
“We are constantly re-evaluating and comparing devices. About a year ago, we began evaluating the SafeSeal versus manual compression alone to determine if the patch does indeed speed up hemostasis and by what degree,” said Craig Narins, M.D., associate professor of medicine and surgery, divisions of cardiology and vascular surgery.
While the trial data is still in the analysis stage, initial impressions of the SafeSeal are very favorable, says Dr. Narins. It allows for the removal of sheaths, even larger sizes, at higher ACT (active clotting time) levels, which means patients can ambulate sooner. Complete trial data should be in publication by the end of the year, Dr. Narins projects.
“Our staff was initially very skeptical that these patches that don’t even contact the artery would work. We found, however, that the artery seals off in under 15 minutes the majority of the time, even at higher ACT levels,” he said.
While not a replacement for vascular closure devices, Dr. Narins believes hemostasis patches definitely have a role in the cath lab and represent a good alternative when use of a closure device is not advisable.
Room for Improvement
Vascular closure technology is a fairly recent development and while there have been many advancements so far, the search for the ideal device continues.
“Today’s vascular closure devices are designed for 6-7 Fr sheaths, although they may be pushed to an 8 or 9 Fr. As a result, I believe there is big need for devices than can close larger holes required for procedures like endografting and aneurysms, etc.,” said Dr. Ramaiah.
Dr. Kim believes there is room for improvement in the areas of ease of deployment, reducing pain to the patient and further reduction of vascular complication risk, such as acute vessel closure.
According to Dr. Kim, “The ideal vascular closure device would be very effective and very safe, preferably leave no foreign material behind, eliminating the risk of infection and scarring, and would require minimal to no manual compression.”
Feature | May 13, 2008 | Maureen Leahy-Patano
Sealing the Deal at the Access Site
The search for the ideal vascular access management device gives rise to a variety of product options.


 October 07, 2025
October 07, 2025