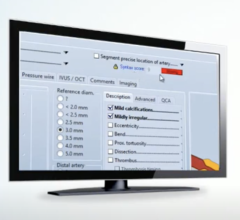
PACS enables surgeons to have immediate access to image information they require for procedures. Photo courtesy of Thinking Systems.
There has been a big buzz circling around the medical community of late about the viability and value of placing PACS into operating rooms (OR) and intensive care units (ICU). Numerous studies have been published in recent years about many of the benefits associated with this newest wave of technology application. One of the most important benefits generally mentioned is that a PACS reduces the amount of time required to obtain necessary radiographic information. In other words, clinicians have more immediate access to the radiographic information they requested for their patients and procedures.
More efficient and expedient access to clinical information frequently translates into better decision-making for the clinicians and shorter lengths of stay for patients. Reducing and eliminating film usage also is frequently cited as one of the great reasons for moving forward with a PACS environment within these critical care areas. These pluses would seem to be a win-win situation for everyone. For sure, proponents for PACS deployment into the OR and ICU are growing daily. The problem is that the “ideal” usage of PACS in the OR/ICU is not always as achievable as it may first appear.
Without a doubt there are a lot of clinicians and radiologists who see merit in the concept of expanded PACS usage. That said, deploying PACS in the OR or the ICU is not the same as deploying PACS within the radiological department or many of the other noncritical care areas. A successful venture into these critical care areas requires careful attention to the operational nuances of these locations so that the surgeons and other technology users have a PACS solution that fits within the scope and limitations of these environments.
For instance, the sterile working environment of the operating surgeon presents a number of unique challenges for normal PACS usage. Additionally, critical care areas are traditionally limited in available space for adding technology, especially applications that require a myriad of functional activities that need to be performed by surgeons and other similar caregivers.
Lighting is also often an issue that has to be dealt with properly within an OR setting. The ability to adequately view images can be severely hampered by inattention to lighting components that are a normal part of this critical care setting.
Can these limitations for deployment be overcome? Yes, especially if the surgeons and critical care staffs are intimately tied to the PACS assessment and implementation process from beginning to end. Likewise, a successful installation of PACS into these environments should have maximum participation from the related radiologist as well.
Another important component of successful PACS implementation within an OR/ICU is the quality of the training related to the technology installed. Critical care areas tend to be high stress environments with limited “spare” time due to the nature of the patient populace. For instance, an area that typically has high unit occupancy and a wide range of severe illnesses often correlates to significant workload constraints for the attending physician. The ability to use the PACS-related technology effectively under these types of working conditions necessitates a much higher quality of training in the use of the PACS workstations and related functional toolsets.
Quality training also lends itself to the wider and more willing use of the technology amongst the providers. As with most technology implementations, the better the integration of the training within the overall project, the greater the overall satisfaction will be toward the end goal.
Audie Lewis is president and CEO of Audie Lewis Consulting, Inc., an independent research and consulting firm serving the healthcare industry. His consulting firm specializes in writing business plans for expansion or emerging operations and in assessing the return on investment value of health care technologies and the successful implementation of related projects. He is a best-selling author whose latest book is Streamlining Health Care Operations: How Lean Logistics Can Transform Health Care Organizations (AHA Press and Jossey-Bass Publishing). He can be contacted at [email protected].


 November 06, 2025
November 06, 2025