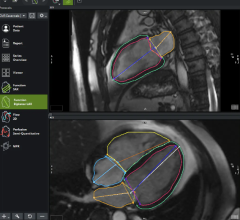
A 3-D printed aortic root with an simulated implant of an Edwards Sapien TAVR valve. New clinical data points to length-of-stay as a new predictor of outcomes in TAVR patients. Image from Henry Ford Hospital.
May 14, 2018 – A new study finds patients who stay in the hospital for more than 72 hours when undergoing trans-femoral transcatheter aortic valve replacement (TF-TAVR) procedure may be associated with negative short and long-term outcomes. The authors, for the first time, report a significant decline in the rates of delayed discharge; and identified independent predictors of both delayed and early discharge post TAVR. The study was presented as late-breaking clinical science at the Society for Cardiovascular Angiography and Interventions (SCAI) 2018 Scientific Sessions.
More than 5 million Americans are diagnosed with heart valve disease each year.[1] TAVR is a procedure used for patients (at high or intermediate risk for surgical aortic valve replacement) with severe narrowing of the aortic vessel where a prosthetic valve is implanted and the damaged valve is replaced. While the strategy of early discharge is important from administrative and financial view point; such practice, may also come with additive clinical benefit in terms of improved short and long-term outcomes. Hence, the aim of this study was to investigate the trends, predictors, and outcomes associated with length of stay (LOS) post TF-TAVR.
Patients undergoing non-aborted transfemoral TAVR, (n=32,847) and survived to discharge (n=24,285) in the Transcatheter Valve Therapy (TVT) Registry from 2011-2015 were categorized as early discharge (ED<72 hours) or delayed discharge (DD). During the study period, there was a significant decline in the rates of DD (62.2 percent in 2012 Q1 versus 34.4 percent 2015 Q3). The study for the first time delineates distinct independent predictors of early/late discharge (multi-variate analysis). said Siddharth Wayangankar, M.D., University of Florida, who presented the study, claims LOS may have immense impact on future care for aortic stenosis patients.
The study also compared one-year outcomes based on LOS. DD post TAVR was significantly associated with higher 1-year all-cause mortality with separation of curves noted immediately post procedure. Even after adjusting for in-hospital complications, DD was an independent predictor of one-year all-cause mortality.
“The predictors from our study could have a huge impact on future clinical care of TAVR patients.” Wayangankar said. “Pre-TAVR, these predictors could be used to develop bedside risk scores for LOS. These could help physicians in patient selection, procedural and post-procedural planning based on patient-specific variables. On a much bigger front, these risk scores could be used by administrators, third-party payors and policy makers for formulating coverage for TAVR procedures and evaluating bundle payments.”
Wayangankar believes the study results have immense post-TAVR implications too. Considering the strong association of DD and outcomes at one year; patients with DD may require a more rigorous follow up schedule to mitigate the higher mortality and hospitalization rates.
The authors note that data from their study (predictors) should be prospectively validated within the TVT registry. Once validated, LOS calculators could help streamline TAVR programs across the world and would help make aortic stenosis care efficient, optimized and sustainable.
Complete listing of SCAI 2018 late-breaking trials with links to articles.
Reference:


 November 14, 2025
November 14, 2025