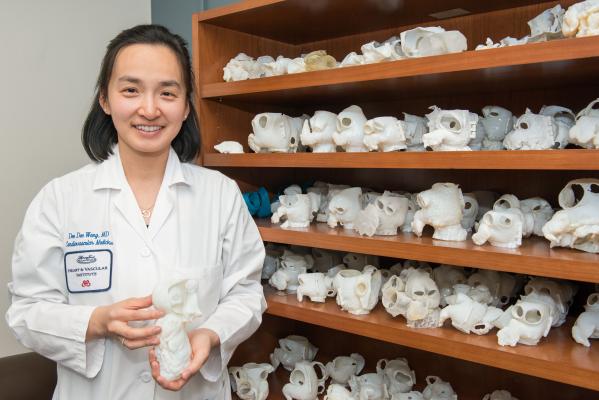
Dr. Dee Dee Wang with part of Henry Ford Hospital's collection of 3-D printed hearts used for education and to preplan structural heart procedures.
March 3, 2017 — A Henry Ford Hospital study found a 100 percent success rate in left atrial appendage (LAA) occlusion procedures when 3-D imaging was used instead of traditional 2-D imaging, the Journal of American College of Cardiology has reported.
When 3-D imaging is used, the procedure also boasts a zero percent complication rate compared to a national average of 16.3 percent rate of serious complications in previous clinical trials using 2-D imaging, according to the study led by led Henry Ford Hospital cardiologist Dee Dee Wang, M.D. The study was published Nov. 21 online in JACC: Cardiovascular Interventions, a publication of the American College of Cardiology Foundation. It looked at the implantation of a LAA closure device, a procedure that lowers the risk of stroke in patients with atrial fibrillation.
Wang and the team at the Henry Ford Center for Structural Heart Disease also found 3-D imaging decreased the length of the LAA procedure by 34 minutes, which allows for quicker patient recovery and decreases complications.
“These results show just how impactful advanced 3-D imaging is to medicine,” said Wang, who was recently named medical director of 3D printing at the Henry Ford Innovation Institute. “The pre-planning results in fewer last-minute decisions, less contrast usage, and less catheter movement inside the heart, thereby minimizing the risk of complications. This is the ultimate in personalizing care for our patients.”
Transcatheter Occulsion of the LAA
The condition – misfiring by the electrical impulses in the upper chambers of the heart – affects how the heart beats and the flow of blood through the body. Due to the irregular and chaotic rhythm, blood can pool, forming clots in a small pouch of the LAA. That raises the risk of stroke five times higher in people with atrial fibrillation, according to the American Heart Association.
The most common treatment to reduce stroke risk in patients with atrial fibrillation is blood thinners. Despite the proven efficacy, long-term use of blood thinners is not well-tolerated by some patients and carries a significant risk for bleeding complications. Researchers say nearly half of atrial fibrillation patients eligible for blood thinners are currently untreated due to tolerance and adherence issues.
Approved by the FDA in 2015, the Watchman device closes off the left atrial appendage, dramatically reducing the risk of stroke and alleviating the need for blood thinners. In about an hour, doctors insert a catheter through a leg vein and into the heart, then open the Watchman device to seal off the left atrial appendage sack. Following the procedure, patients typically need to stay in the hospital for 24 hours. Most patients will be able to discontinue the use of blood thinners after 45 days.
Key to the procedure is anticipating the twists and turns of the heart to reach the LAA, then choosing the correct size Watchman device to seal the opening.
In the study between May 2015 and February 2016, the Henry Ford Center for Structural Heart Disease team implanted the Watchman in 53 patients. All patients underwent pre-procedural CT imaging of the LAA, followed by intraprocedural echocardiographic characterization and guidance with 2-D and 3-D transesophageal echo (TEE) imaging.
In a previous national study, cardiologists using 2-D imaging to insert the Watchman used an average of two devices (1.8 devices per implantation attempt) as they tried to perfectly match the size of the device and the appendage’s opening. But when the Henry Ford cardiologists used 3-D imaging in this most recent study, they were able to size the Watchman device accurately in nearly 100 percent of the procedures (1.245 devices per implantation attempt).
They Henry Ford team also found that they were able to help more patients qualify for this procedure with 3D imaging than 2D. By traditional 2-D imaging, 10 of the 53 patients (18.9 percent) would have been turned down inappropriately for a procedure they could have benefitted from due to operator inability to fully visualize their anatomy.
“Using 3D imaging allows the doctor to ‘see’ into the heart,” Wang explains. “This is especially important when planning how to move through the left atrium, anticipating the complexity and size of a left atrial appendage.”
Long-time pioneering cardiologist William W. O’Neill, director of the Center for Structural Heart Disease, said the study reinforces the importance advanced work being done at Henry Ford.
“We pride ourselves on offering life-saving treatments to patients – some who have been told they have no other options,” O’Neill said. “The 3-D Imaging allows us to do it safer and more efficiently. This study also shows why other centers who are not as experienced as our team should absolutely be using this technology to help patients.”
For more information: www.henryford.com/heart

 May 12, 2020
May 12, 2020 









