May 13, 2014 — The Heart Rhythm Society (HRS), American College of Cardiology (ACC) and American Heart Association (AHA) released Expert Consensus Statement on the Use of Implantable Cardioverter Defibrillator Therapy in Patients Who Are Not Included or Not Well Represented in Clinical Trials at Heart Rhythm 2014, the 35th annual scientific sessions of HRS. The expert consensus statement provides first-of-its-kind guidance on ICD therapy for the management of patient populations who are not well represented in clinical trials and, as a result, not specifically included in existing guidelines.
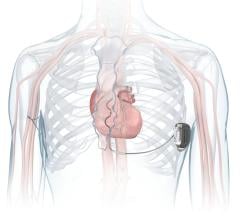
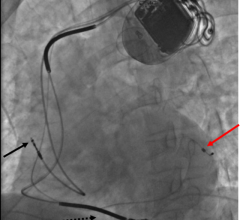
ICDs have emerged as an important treatment option for patients who are at risk of sudden cardiac arrest, and are very effective for stopping life-threatening abnormal heart rhythms. However, while ICD therapy has been proven beneficial in many patient populations, there remain scenarios where clinicians are often asked to make decisions regarding ICD therapy for patients who fall outside of existing guidelines.
"Without exception, guidelines help clinicians make important decisions when it comes to ICD therapy; however, we must continue to refine our understanding of who benefits from ICD implantation in order to optimize patient care," said task force chair and lead author of the statement, Fred M. Kusumoto, M.D., FHRS, the Mayo Clinic in Jacksonville, Fla. "Because guidelines are mainly determined by the outcomes of large clinical trials, smaller patient populations or unique circumstances are typically not provided with indications for treatment. This document will serve as a new guide for clinicians so that many more, if not all, patients receive the right treatment at the right time."
The members of the writing group performed a comprehensive literature search, and then developed a series of recommendations with an explanation of the reasoning and research used to make each recommendation. The writing group also evaluated the available data on important situations for which ICD therapy might be beneficial in selected populations.
The expert consensus statement includes specific recommendations for the following four situations:
- Use of an ICD in patients with an abnormal troponin that is not due to a myocardial infarction (MI);
- Use of an ICD within 40 days after a MI;
- Use of an ICD within the first 90 days after revascularization; and
- Use of an ICD in the first nine months after initial diagnosis of nonischemic cardiomyopathy.
Additionally, the writing group evaluated the utility of an atrial lead in a patient requiring ICD therapy without cardiac resynchronization therapy (CRT). The statement provides recommendations for specific scenarios where CRT is not indicated or not desired and a clinician must decide between a single- or dual-chamber ICD. Specific scenarios, including but not limited to those with AV block, Long QT syndrome, and persistent or permanent AF, are outlined with atrial lead use noted as either recommended, not recommended, can be useful or may be considered.
The recommendations aim to help improve consistency and overall quality among hospitals and healthcare providers. Initiatives that standardize data elements and define best practices are critical for leveraging the benefits of ICD therapy to large populations. Future research should continue to evaluate the effectiveness and value of ICD therapy.
The consensus statement was developed in collaboration with and endorsed by the Heart Failure Society of America (HFSA) and the Society of Thoracic Surgeons (STS). It was endorsed by the European Heart Rhythm Association (EHRA), Asia Pacific Heart Rhythm Society (APHRS) and Latin American Society of Cardiac Pacing and Electrophysiology, and will be published in the July 2014 edition of HeartRhythm.
For more information: www.hrsonline.org


 January 13, 2026
January 13, 2026