There is a trend in interventional cardiology that is now being called “renalism,” where patients with poor renal function are being excluded from interventional procedures because they are automatically considered too high risk. However, some hospitals are also creating cardio-renal care teams so these patients can be cared for by a team of experts rather than interventional cardiologists going it alone.
There is a trend in interventional cardiology that is now being called “renalism,” where patients with poor renal function are being excluded from interventional procedures because they are automatically considered too high risk. The fear is using angiographic contrast may cause contrast induced nephropathy (CIN) or serious kidney injury resulting in these patients going on dialysis. However, these patients can be treated using some unconventional approaches to reduce or eliminate contrast use. Some hospitals are also creating cardio-renal care teams so these patients can be cared for by a team of experts rather than interventional cardiologists going it alone.
This trend of excluding patients is partly driven by some states having public reporting requirements for quality metrics, and most cardiologists do not want to have have it public that they cause patients to go on dialysis, explained Ziad Ali, M.D., director of the DeMatteis Cardiovascular Institute, director of investigational interventional cardiology, and director of the cardio-renal program at St. Francis Hospital and Heart Center in New York. He is also director of the Angiographic Core Laboratory at the Cardiovascular Research Foundation (CRF).
He helped start a cardio-renal program at Columbia University Medical Center and St. Francis Hospital. He spoke on this experience at the Society of Cardiovascular Angiography and Interventions (SCAI) 2021 Scientific Sessions.
"I had a patient that had a GFR12 and did my first zero-contast PCI in 2015. I had every intention of taking a final angiogram when at the end of the case a nurse asked me if I was going to take a picture," Ali said. "I looked over at her and said 'no.' I already IVUSed it and the stent apposition was perfect, and I did post PCI FFR and the FFR was normal. So I asked myself what value will this final picture have. I just pulled the wires out and that was it. And that is how the program really started."
In 2016, the team at Columbia published the article "Diagnosis and Management of Cardiovascular Disease in Advanced End-stage Renal Disease"[1] which serves as a guide on how to create a cardio-renal program.
Ali explained patients with end-stage renal disease (ESRD) account for 53 percent of deaths with known cause for patients with heart disease. The exclusion of these patients in randomized controlled trials has led to a lack data, making the cardiovascular management of these patients very challenging. But, there are patients who can benefit from various intervention and can have good outcomes if they are managed properly.
"There is this imminent need for specialists in this area," Ali said. “ESRD is common and the outcomes in these patients is poor."
For these reasons he said creating a cardio-renal program makes a lot of sense so patients with poor renal function and be included in interventional therapies by allowing a greater safety net with a team of experts available to screen, plan the procedure and care, and quickly help with any complications.
Creating a Cardio-renal Care Team
Ali explained the first step in creating this type of program is putting together the required sub-specialists who have interest. He said this not something you can do by yourself and it requires a team effort to care for these patients. Team members should include:
• General cardiologist (established care)
• Preventive cardiologist (hypertension, hyperlipidemia)
• Heart failure cardiologist (HFpEF, HFrEF, high output)
• Interventional cardiologist (CHIP)
• Electrophysiologist (AICD strategies)
• Pulmonary Hypertension Specialist (high output, systemic HT)
The general cardiologist can help coordinate things with these patients, because there are a large number of them.
The preventive cardiologist can help with their difficult to control control hypertension, hyperlipidemia. Despite many of these patients having low LDL on blood tests, this is usually because they are excreting large amounts of LDL in their urine and not because they actually have low LDL. So the specialist can help monitor this and ensure these patients are on a statin.
“You need a heart failure cardiologist who really knows HFpEF, because all these patients have had years of hypertension and their ventricles are like wooden boxes. You also have a lot of patients with reduced ejection fraction and ischemia," Ali said. "And then there is this huge problem with high output due to AV fistulas."
Ali said the interventional cardiologist needs to be very good and this program and these patients are not something you dabble with. "You need someone who is facile with complex wires, complex calcium management, intravascular imaging and advanced physiology," he explained. Ideally, this person should be an operator involved in high-risk indicated percutaneous coronary interventions (CHIP).
The electrophysiologist needs to be someone who understands you cannot just place an implantable device in every patient with reduced ejection fraction because these patients get a dialysis needle stuck in their arm three times a week and their infection risk is very high.
He said getting a pulmonary hypertension specialist might be the hardest person to find. These renal patients often have high output failure and they often have extremely high systemic hypertension, so you need someone who can separate systemic from pulmonary pressures.
Creating a Standardized Clinic Template and Clinical Pathway for End-stage Renal Disease Patients
Ali said it is important to create a standardized clinic template report so everyone is asked the same questions and it is easy for the referring doctor to know what you are looking. This also helps with creating a detailed database that can be used prospectively to assess patient characteristics and outcomes.
They also created a pathway document for these patients that outlines what should be done to minimize renal impact. He said there is no consensus on the optimal noninvasive imaging approaches for these patients, so they created their own rules.
SPECT and echo are the usual go-to cardiac imaging exams, but both have issues with reduced sensitivity in ESRD patients. However, Ali said they found positron emission tomography (PET) can also assess coronary flow reserve (CFR), which they found offers insights into early stage microvascular dysfunction and heart disease. PET also has been shown in recent studies to provide incremental risk stratification for cardiovascular disease and all-cause mortality in patients on renal replacement therapy (RRT), even in the absence of overt cardiovascular disease.
He said this may be an issue for many hospitals that do not have access to PET imaging, but this is what they use as a first-line stress test imaging modality.
If a patient has any evidence of reversible ischemia on stress testing, angiography and revascularization should be performed.
Revascularization of ESRD Patients
Ali said revacularization of patients with PCI prior to renal transplant improved the 5-year outcomes in these patients post-transplant compared to those medically managed. He also said PCI and surgical coronary artery bypass grafts (CABG) in patients with ESRD show similar long-term outcomes. For those reason, it is good to have a cardiac surgeon as part of the team who understands the complexity of these patients.
"This population is totally different from the patients in the COURAGE and SYNTAX data, they are sort of an alien population," Ali explained.
For PCI, he said drug-eluting stents are the way to go, because this population already has a higher restenosis rate than the general population, Ali said. He said these patients have double the restenosis rates, at about 20 percent of cases. Bare metal stents should be avoided for this reason.
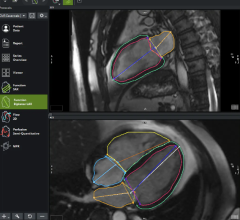
PCI procedures should be performed using intravascular imaging guidance rather than angiography. This will reduce or eliminate the need for contrast in the renal-compromised patients. This can include intravascular ultrasound (IVUS) or optical coherence tomography (OCT).
Ali said he uses a post-procured FFR and IVUS of the vessel segment to verify a PCI is successful, rather than doing a final angiogram.
Heart Failure And Other Pitfalls in Management of ESRD Patients
About 36 percent of patients initiating RRT have heart failure, a rate of 12 to 36 times the general population, Ali explained. And about 25 percent of patients on RRT develop de novo congestive heart failure.
Use of ACE-I and beta blockers (BB) have variable results in this population, but Ali said meta analysis show BB therapy lowered all-cause and cardiovascular mortality.
Renal transplant has been shown to halt the progression of congestive heart failure.
Left ventricular hypertrophy (LVH) and fibrosis in these patients also increased the risk of developing left ventricular dysfunction and ventricular arrhythmias. This can open patients to higher incidence of sudden cardiac death (SCD).
Despite this, Ali said there is little evidence showing implantable cardioverter defibrillators (ICDs) are useful in this population. He said these patients are also at a much higher risk of infection, especially in patients with trans venous leads into the heart. That infection risk may be higher than the risk of SCD, Ali said. For that reason the EP involved with the team should be facile with subcutaneous ICD implants to minimize infection risks.
Valvular disease with heavy clarification is very prevalent in these patients as well. This often poses a barrier to transplantation.Degenerative vault calcification also progresses faster in ESRD patients. Premature development of aortic stenosis is also associated with longer time on RRT.
Dialysis patients also have extreme variability with their aortic or mitral regurgitation because on when they had RRT last. Ali said patients who just had RRT will have low volumes a their regurgitation volumes will be lower, but the next day the volume and regurgitation will be much higher. It is important the team treating this patient understands this variability. To monitor this he said you need to use what is known as a "dry" echo on the day of their dialysis.
"Pulmonary hypertension is a real challenge, and this is often caused by the patients AV fistula, which leads to high output," Ali said. Management really requires a pulmonary hypertension specialist.
Management of patients with severe systolic dysfunction is another big problem in these patients.
Including Renal Compromised Patients Can Increase Cath Lab Procedure Volumes
“This is a very good way to increase your patient volumes if you are dedicated to create these types of programs,” Ali said.
After implementing the cardio-renal program at his center, Ali said total invasive procedures per yer went from about 450 to between 600 and 700 per year.
Non-contrast PCI is Possible in ESRD Patients
“I like to apply the idea we use in imaging with the ALARA principle, which stands for as low as reasonable achievable,” said Ashish Pershad, M.D., an interventional cardiologist at Dignity Health Medical Group Cardiology, Mercy Gilbert, in Gilbert, Ariz. He spoke at SCAI 2021 on strategies to reduce or eliminate contrast in renal compromised patients, even if you do not have advanced imaging technologies.
He recently transitioned jobs from a large academic center at Banner Health in Phoenix, to a community hospital program that does not have all the fancy technologies to help navigate interventional procedures. He offered a list of real-world ideas for how smaller hospitals can reduce or eliminate their use of contract in these select patients. He said some things that can be done are very simple, such as using a printed picture of a patient’s angiogram from another hospital and taping it to the main overhead screen to act as a guidance tool on non-contrast fluoro. He also said IVUS can be used an alternative imaging modality for stent sizing, lesion length and to identify landing zones. He also wires the vessels with very radiopaque wires to aid vessel navigation.
“We are creatures of habit and we need to break this habits to be able to help our patients,” Pershad explained. “We also need to get the word out about ‘renalism,’ but the biggest issue is the need to educate our own audience of cardiologists,”
Related Content on Reducing Kidney Injury:
Understanding Contrast-Induced Nephropathy
VIDEO: Strategies to Avoid Acute Kidney Injury Caused by Cath Lab Contrast — Interview with Roxana Mehran, M.D.
Sliding Scale Hydration Washes Out Contrast-Induced Kidney Complications
VIDEO: How to Avoid Acute Kidney Injury in the Cath Lab — Interview with Hitinder Gurm, M.D.
Contrast-Induced Kidney Injury Prevented With RenalGuard in REMEDIAL III Trial
VIDEO: Combating Contrast Induced Nephropathy in the POSEIDON Trial — Presentation by Sonjot Brar, M.D.
New MRI Technique Spots Heart Muscle Scarring Without Kidney Damage
No Benefit Found Using Sodium Bicarbonate, Acetylcysteine to Prevent Kidney Injury
Strategies to Lower CT Contrast Dose and Track Usage
DyeMINISH Multi-center Global Patient Registry Launched
Reference:


 November 14, 2025
November 14, 2025