March 15, 2015 — Patients who received the new drug Bendavia before undergoing angioplasty or stent implantation after a heart attack showed no significant reduction in scarring compared to patients given a placebo, according to a new study.
Patients who received the new drug Bendavia before undergoing angioplasty or receiving a stent to clear blocked arteries after a heart attack showed no significant reduction in scarring as compared to patients given a placebo, according to a study.
The study — presented at the American College of Cardiology’s 2015 Annual Scientific Session — is the first randomized, controlled trial of Bendavia, a drug designed to reduce the extent of tissue damage in the heart through a new approach that targets mitochondria in the cells. Although patients receiving the drug showed a 10 percent reduction in scarring during the first three days after surgery as measured by the levels of an enzyme called creatinine kinase-MB, the study’s primary endpoint, the difference was not statistically significant. The results also suggested a trend toward improved heart pumping function during the eight hours following the drug’s administration, but that trend also did not reach statistical significance.
“Our study found that the drug did not prevent irreversible injury to the heart,” said C. Michael Gibson, M.D., professor of medicine at Harvard Medical School and the study’s lead author. “However, we did see a trend for patients to have a reduced incidence of new onset heart failure in the first eight hours after the infusion, which may indicate that Bendavia could help improve heart pumping function for heart failure patients. This hypothesis-generating observation is being prospectively evaluated in an ongoing study.”
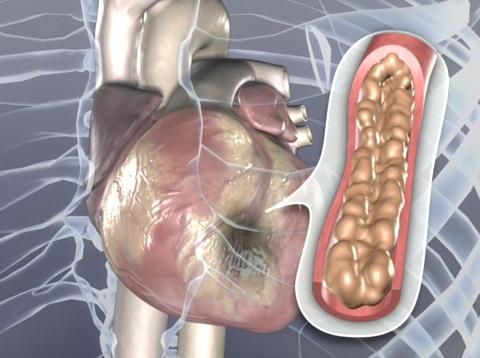
Bendavia, which showed promise in animal studies, was developed to improve outcomes for patients who suffer a heart attack and undergo stenting and angioplasty, a procedure in which a surgeon threads a device through a vein in the groin or arm that is then inflated or expanded to open the artery and allow blood to flow through. Angioplasty is performed in more than one million people in the United States each year.
Patients who undergo angioplasty after a heart attack typically have permanent tissue damage and scarring in the heart, up to half of which can be attributed to the injury that occurs as a result of restoring blood flow in heart tissue that has been deprived of oxygen, a process called reperfusion injury. This damage causes the heart to work harder to pump blood and increases the likelihood of future heart failure.
Bendavia uses a new approach to reduce the extent of angioplasty-related injury and scarring by bolstering the cells’ natural systems of energy production during the procedure. “The mitochondria—the powerhouse of the cell—is one of the key players in reperfusion injury,” Gibson said. “The goal of Bendavia is to help the mitochondria stay functional and therefore to reduce the amount of tissue damage and injury.”
Bendavia’s activity in the mitochondria could also help it improve heart function for people with heart failure.
“For patients with failing hearts, we currently give drugs that make the heart pump harder, increasing the demands on the heart,” Gibson said. “By contrast, this drug aims to supply more energy to the cells to improve the supply side of the equation, which is a different approach.”
The trial included nearly 300 patients at 24 hospitals in four countries who underwent angioplasty and stenting after ST-elevation myocardial infarction, the most severe type of heart attack. Half of the patients were randomly selected to receive a placebo and half received a dose of Bendavia starting at least 15 minutes before their procedure. The drug and placebo were infused via intravenous drip over the course of one hour.
The results fell short of statistical significance for all primary and secondary endpoints that were identified for the study, which included the size of the damaged heart tissue as measured by the creatinine kinase-MB enzyme for the first three days, as well as a variety of other common measures of heart tissue damage such as magnetic resonance imaging (MRI), troponin levels and ST-segment resolution.
The results also revealed no difference in clinical outcomes including congestive heart failure, subsequent hospitalization and death, and the drug was not associated with any adverse reactions or safety concerns. The study’s main limitation is that it did not include enough patients to detect a difference as small as 10 percent with statistical significance, Gibson said.
A separate study is currently underway to assess the potential benefits of ongoing Bendavia use in patients with heart failure.
The trial was funded by Bendavia’s developer, Stealth BioTherapeutics.
For more information: www.acc.org


 February 03, 2026
February 03, 2026 









