Artificial intelligence’s (AI) applicability in cardiac imaging is rapidly growing and was a major topic of discussion at this year’s EuroPCR 2022 meeting. Many session speakers discussed how they are using AI tools in their day-to-day practice and in their research to improve decision-making and patient/research outcomes. It’s no secret, however, that AI tools are only as good as the data sets and the thousands of expert opinions used to power them.
Implementing AI applications in our day-to-day practice, from an operations standpoint, could mean adjusting clinician workflows and setting aside time to set up and train on the new systems. And from an efficacy standpoint, it leaves clinicians wary of result accuracy, especially if they are unsure how good the data used to power the technology really is. However, a good AI tool enhances workflow, has a proven ROI and is trained using data samples representative of our population and a variety of expert opinions. When it comes to interpreting and analyzing cardiac imaging, artificial intelligence should seamlessly provide clinicians with an immediately available second opinion, without jumping through hoops or doubting its accuracy. For intravascular optical coherence tomography (IVOCT), AI, when applied correctly, has the potential to aid imaging technology adoption rates, improve decision-making and patient outcomes.
I started my company, Dyad Medical, to help address the challenges cardiology experts face. We develop clinical applications that use cloud-based AI technology to enable clinicians and researchers to interpret medical images more efficiently and accurately. We focus solely on cardiac imaging because more people die as a result of cardiovascular disease than all types of cancers, diabetes and accidents combined. Our aim is to arm clinicians and researchers with AI-powered tools that provide them with immediately available second opinions to enhance their practice.
We would not be developing these solutions without the challenges we experience in our field, however. Many studies suggest adopting imaging technology promotes better patient outcomes, but the major barriers are the need for learning specific image analysis skills and more time, that we simply do not have, to manually analyze images. I believe we can use AI to overcome these barriers, but we still need to fully understand why imaging modalities are not being used to their full potential and the limitations of AI in our field.
Intravascular OCT Adoption Rates
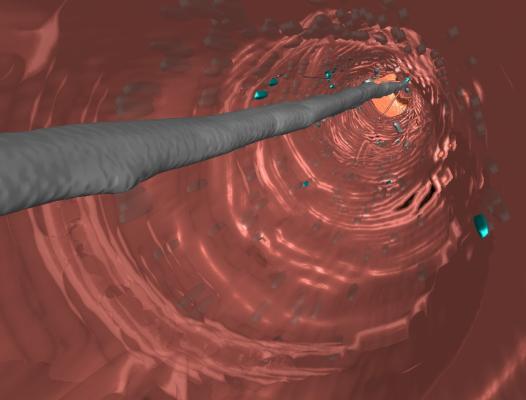
Today, high-resolution intravascular imaging guidance helps reduce adverse cardiac events by optimizing stent implantation and mitigating structural risk factors for stent failure. IVOCT offers better image quality and therefore very accurate measurements. IVOCT’s high resolution makes it easier to evaluate stent strut apposition against vessel walls. It is the lone imaging modality with the resolution and contrast able to optimize stent design.
However, despite improved patient outcomes, intravascular imaging remains severely underutilized in clinical practice. IVOCT requires a great amount of interpretation skills to understand the nuances of cardiac images. Until now, IVOCT imaging adoption rates have been hampered, especially among less experienced clinicians, because image interpretation requires operators to be proficient in manual image analysis and to be able to interpret a large amount of data in real-time. As a result of these challenges, intravascular imaging clinical decisions are often based on insufficient and/or incomplete data.
The Breaking Point — Time and Expertise Shortage
We are hitting a breaking point with imaging technology where the minor improvements to the current standards of manual analysis succumb to the pressures of time. On top of that, disagreement among experts, diagnostic error rates and a shortage of professional experts become more prevalent as burnout runs rampant in labs, health systems and private practices.
Even for trained experts, the current fast-paced clinical workflow precludes comprehensive evaluation of intravascular images during the procedure, a process that can require hours of manual labor to complete. At present there are no existing clinical software tools that can perform comprehensive automated intravascular image analysis.
Trust Built on Data
While we understand the practical and operational barriers to imaging technology and AI tool adoption, above all, we must be able to trust that the technology we’re using is based on evidence. AI programs must be trained on high quality data, be stringently vetted and built on expert insights. AI technology is by no means perfect, and it’s important to note that perfection isn’t the end goal. But to trust the accuracy of the AI tool, we have to look deeper at the data set and the expert opinions driving image analysis.
Today’s fast-paced clinical environment demands we treat more patients in less time. In our highly technical and highly specialized field, analyzing images quickly inevitably leads to mistakes, burnout and disagreements among experts. Advancements in technology can help ease the burden, but can we rely on these high-tech tools to produce better results for our patients?
The uncertainty lies in not knowing the quality of data used to train the AI tools.
This all boils down to two criteria: 1) training the AI tool with representative data samples; and 2) relying on many expert opinions.
First, our data samples should be representative of the patients we serve. For example, if the AI imaging tool is intended for use in the United States, the images we are analyzing to power the tool should come from a diverse pool of patients of different demographic backgrounds, similar to the makeup of the U.S. population. This includes different age groups, physical attributes like height and weight, medical history such as surgeries and medications, genetics like family history of heart disease, and other variables that impact a patient's overall health.
Second, the expert analyses should come from many different sources. Ideally, we’d be able to analyze images objectively and not let bias get in the way. The reality is, we each have a unique way of approaching our work and disagreement among experts is bound to happen. That’s why relying on many opinions is paramount to training an AI algorithm. The more expert opinions powering the AI, the better overall accuracy of the analyses.
AI Becoming an Integral Part of Value-based Care
Healthcare costs for cardiovascular diseases is expected to reach $1.1 trillion in 2035. These escalating costs are partly due to the shortage of cardiologist specialists, high workloads and burnout. AI that helps solve these problems can help improve patient outcomes and reduce overall healthcare costs.
Addressing workflow inefficiencies and finding opportunities to automate time-intensive tasks is the challenge of today. AI will not replace clinicians, but it is improving the process of treating patients. For cardiac imaging, this means the AI technology of tomorrow will substantially decrease misdiagnosis and expert disagreement, minimize healthcare costs by integrating it into workflows and provide universal access to thousands of second expert opinions. The end result is the support clinicians and researchers need to make decisions and draw conclusions that will improve patient outcomes and drive down costs of care.

Ronny Shalev, Ph.D., is CEO and founder of Dyad Medical Inc., a company that develops FDA-cleared software which automatically analyzes the content of cardiac and cardiovascular images using artificial intelligence. He has spent much of the past 25 years in executive positions, including VP of Sales and Marketing at Orbotech, where he managed teams of >100 people worldwide and Director of the World-wide Program Management at Marvell Semiconductor. An expert in developing new projects, medical image processing, machine learning and visualization, he has a significant amount of experience as an entrepreneur and is dedicated to using his skills to help physicians make accurate decisions to improve patient outcomes. He holds a Ph.D. in electrical engineering and computer science from Case Western Reserve University.
Related AI Content:
Viz.ai Launches Two New AI-Powered Modules for Pulmonary Embolism and Aortic Disease
VIDEO: Artificial Intelligence Trends in Medical Imaging — Interview with Sanjay Parekh, Ph.D.
GE Healthcare Receives FDA Clearance for First X-ray AI to Help Assess Endotracheal Tube Placement
RSNA Announces Results of Brain Tumor AI Challenge
AI Gut-imaging Software Takes on the U.S. with FDA Clearance and National Hospital Partnership


 January 28, 2026
January 28, 2026 









