The ubiquitous smartphone has found its way into the pockets of nearly every clinician and patient in recent years and offers new opportunities to greatly redefine healthcare in the coming years. Smartphones and apps for healthcare — referred to as mobile health or mHealth — offer a key technology to help reduce healthcare costs, improve the efficiency of care delivery and enable greater access to high-quality care via telemedicine. mHealth can serve as a bridge between providers, healthcare IT and patients to enable true patient engagement. These tools also can help empower patients to take more responsibility for their own health and offer the ability to interface and collaborate more with their providers.
There are now about 165,000 published mHealth apps available,[1] and the U.S. Food and Drug Administration (FDA) recently developed guidelines for regulating the small fraction of these clinical-grade apps. Today, these apps enable patients to use their phones to track their fitness, record calorie and diet information, heart rate and single lead ECGs, enter medication reminder alarms, manage diabetes, and even access their lab results, reports and imaging from their electronic medical records (EMR). Proponents of mHealth say this is just the tip of the iceberg for the potential of apps and mobile devices to impact the future of healthcare.
Read about the "Uberization" of healthcare
Future of Apps in the Next Five Years
Key trends and app usage in mHealth have been tracked since 2010 in a large annual survey by the market intelligence firm Research2Guidance, in partnership with Telefonica, the mHealth Summit Europe, Johnson and Johnson, and Novartis. The results of the “mHealth App Developer Economics 2015 — The Current Status and Trends of the mHealth App Market” survey, released last November, had more than more than 5,000 respondents, including healthcare app developers and clinicians.[1]
Researchers found the 165,000 published mHealth apps were downloaded more than 3 billion times in 2015. These apps are composed of two main types - health and fitness apps (i.e. wearable activity monitors or calorie tracker apps) and medical apps (i.e. medical references and FDA-cleared apps used for clinical diagnostics). The breakdown of available mHealth apps includes health and fitness apps as the largest group, making up about 56 percent of what is offered by app stores. The medical app category makes up about 44 percent, with the majority of these being for reference. There are a growing number for chronic disease management, which currently make up about 12 percent of apps. Within that group there are apps that claim to help obesity management (29 percent), followed by diabetes (20 percent) and cancer (19 percent).[2]
Apps that help monitor or manage a patient’s medical condition, enable remote access to patients’ EMRs and remote clinical consultations are all expected to see increased usage. EMR interface apps are now expanding to include bi-directional upload of data and images to doctors’ offices for inclusion in EMRs. This same technology can be leveraged for telemedicine consults.
Respondents said apps for patient follow-up — especially after hospital discharge — and chronic disease management for diabetes, heart failure and hypertension, were seen as the biggest areas of potential impact on healthcare. Since the first survey in 2010, diabetes has been considered the chronic disease area with the highest potential growth for mHealth. Today, 70 percent of mHealth practitioners rate diabetes highest in terms of business potential in the next five years. This is followed by apps to help manage obesity (38 percent), hypertension (29 percent), depression (23 percent) and chronic heart diseases (16 percent).
Survey respondents said the biggest expected impact of mHealth in the next five years will be on patient follow-up monitoring. About 60 percent of mHealth providers said patient follow-up and monitoring via wearables and mobile app interfaces will be a major driver for patient engagement. About 40 percent said the second most popular use of mHealth will be patients leveraging the technology to quickly find health information about their conditions or managing their health.
mHealth providers said automation of data input will become a big trend. Apps are already becoming more connected to sensors to feed in activity, nutrition or biometric data. According to the survey, 70 percent of mHealth practitioners said built-in sensors in smartphones (including accelerometers and heart rate measured with the phone's camera) will likely be the area with highest market potential, followed by wearable devices (53 percent). Wearable devices include wristbands, patches or chest belts that transmit the data wirelessly via Bluetooth or a cable to the smartphone. Sensors that plug into a smartphone, including thermometers, blood pressure monitors and glucose monitors, also are expected to become very popular.
Watch the video "How Wearable Devices Will Fit in Healthcare and Patient Engagement."
Reducing Readmissions, Healthcare Costs
Survey respondents said mHealth apps promise to significantly reduce healthcare costs once integrated into the healthcare system. One area where mHealth is expected to have a major impact is reducing readmissions and the length of stay by allowing remote monitoring of patients at home, rather than have them taking up hospital beds. Another area practitioners said apps will have a major impact in reducing healthcare costs is by cutting medication non-compliance through the use of simple pill reminder apps.
As the aging U.S. population increases demands on providers, survey respondents say apps may help reduce the number of office visits and cut the number of repeat exams via mobile access to the patient’s EMR and with use of use remote diagnostics solutions that interface with the mobile device.
Doctors are also expected to see an impact from apps in the next couple years, as 41 percent of mHealth app publishers and decision makers foresee they will treat their patients, schedule appointments or execute diagnostics using mobile devices rather than by conventional means or workstation computers.
The FDA’s Views on Medical Apps
As the use of mobile devices and smartphones has rapidly proliferated in healthcare, there has been a flood of medical applications (apps) developed for all facets of medicine. In an increasingly tech savvy world, people want information to be at their fingertips when and where they need it via their mobile devices. In 2013, the FDA created a tailored approach to apps that supports innovation while protecting consumer safety, and it updated these guidelines in February 2015.[3] The FDA outlines two categories for regulated and unregulated apps. Unregulated apps include those offering patient education, those that help patients keep track of their health, as well as clinical reference and clinical training. The FDA said it will concentrate its regulatory efforts only on apps that may impact patient safety or that transform the mobile device into a regulated device, such as accessing software that requires FDA 510(k) market approval. This includes accessing picture archiving and communication systems (PACS), or apps that convert the mobile device into a patient diagnostic device, such as an ECG monitor, testing device or ultrasound imaging system.
The FDA stated that patients with diabetes already use FDA-cleared smartphone apps to monitor the level of sugar in their blood, and doctors can often use their tablets to read X-rays and perform ultrasounds or electrocardiograms. The agency said those functions represent just the tip of the iceberg of what it expects to come. The agency created the guidelines to be ready to handle the influx of new apps requiring FDA review.
The FDA said mobile apps have the potential to transform healthcare by allowing doctors to diagnose patients with potentially life-threatening conditions outside of traditional healthcare settings.
“Mobile apps are unleashing amazing creativity, and we intend to encourage these exciting innovations,” said Bakul Patel, associate center director for digital health at the FDA. “At the same time, we have set risk-based priorities and are focusing FDA’s oversight on mobile apps that are devices for which safety and effectiveness are critical.”
Regulating Apps
The FDA intends to exercise enforcement discretion (meaning it will not enforce requirements under the Federal Drug and Cosmetic Act) for the majority of mobile apps, since they only pose minimal risks to consumers. The agency intends to focus its regulatory oversight on a subset of mobile medical apps that present a greater risk to patients if they do not work as intended.
“Some mobile apps carry minimal risks to consumers or patients, but others can carry significant risks if they do not operate correctly. The FDA’s tailored policy protects patients while encouraging innovation,” said Jeffrey Shuren, M.D., J.D., director of the FDA’s Center for Devices and Radiological Health.
The FDA is focusing its oversight on mobile medical apps that:
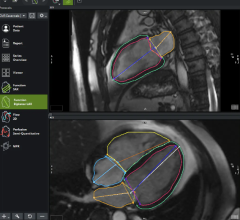
• Are intended to be used as an accessory to a regulated medical device — for example, an application that allows a healthcare professional to make a specific diagnosis by viewing a medical image from a PACS on a smartphone or tablet; or
• Transform a mobile platform into a regulated medical device — for example, an application that turns a smartphone into an electrocardiography (ECG) machine to detect abnormal heart rhythms or determine if a patient is experiencing a heart attack.
The agency said it does not regulate the sale or general consumer use of smartphones or tablets, nor does it regulate mobile app distributors such as the iTunes Apple store or the Google Play store.
Patel explained, for example, that FDA would regulate a mobile medical app that helps measure blood pressure by controlling the inflation and deflation of a blood pressure cuff (blood pressure monitor), just as it regulates traditional devices that measure blood pressure. A false reading by either blood pressure device would deliver a false diagnosis and perhaps even lead to treatment that could endanger patients.
However, although a mobile app that doctors or patients use to log and track trends with their blood pressure is a medical device, as explained in the final mobile medical app guidance, such mobile apps would not fall within the current focus of FDA’s regulatory oversight. Similarly, mobile medical apps that recommend calorie or carbohydrate intakes to people who track what they eat also are not within the current focus of FDA’s regulatory oversight. While such mobile apps may have health implications, FDA believes the risks posed by these devices are low and such apps can empower patients to be more engaged in their own healthcare.
Specific Examples of Regulated Apps
The FDA defines regulated mobile apps as those that are an extension of one or more medical devices by connecting to it for control purposes or displaying, storing, analyzing or transmitting patient-specific medical device data. This includes the remote display of data from bedside monitors or of medical images directly from a PACS server. Other regulated apps include those that transform the mobile platform into a regulated medical device by including functionalities similar to those of currently regulated medical devices. This includes apps that offer a blood glucose strip reader to a mobile platform to function as a glucose meter; attachment of ECG electrodes to measure, store and display ECG signals; or use of sensors on a mobile platform for creating an electronic stethoscope function. Apps that display radiological images for diagnosis also transform the mobile platform into a Class II-regulated PACS, according to the FDA.
The FDA has cleared several mobile medical apps with attachments to a mobile platform. Specifically, patient monitoring apps that monitor a patient for heart rate variability from a signal produced by an ECG, vectorcardiograph or blood pressure monitor are classified as cardiac monitoring software. Other mobile medical apps that use a hardware attachment or interface to a monitoring system that have been cleared include an automatic electronic blood pressure monitor.
Mobile apps that become a regulated medical device by performing patient-specific analysis and providing patient-specific diagnosis or treatment recommendations will also be regulated. Examples include apps that perform sophisticated analysis or interpret data from another medical device, such as apps that calculate dosage or create a dosage plan for radiation therapy; computer-aided detection (CAD) software; image processing software; and radiation therapy treatment planning software. The FDA believes these types of software present the same level of risk to patients regardless of the platform on which they run.
VIDEO: How Wearable Devices Will Fit in Healthcare and Patient Engagement
Read the article, "Understanding How Big Data Will Change Healthcare."
References:







 November 14, 2025
November 14, 2025